In past articles and our most recent article on trauma, we have mentioned the impact that Adverse Childhood Experiences, or ACEs, can have on an individual. While it wasn’t long ago that we figured it out, there is a great deal of research supporting the notion that one of the key contributing factors to substance abuse, mental health and other behavioral disorders is childhood trauma. Adverse Childhood Experiences, known widely as ACEs, are common and seemingly passive experiences that one may have as a child, that, when occurring repeatedly or in combination, have a devastating impact on a person’s development and long-term health.
When an Adverse Life Event takes place during one’s life in later adolescence or as an adult, the connection for the survivor to make between the traumatic experience and their future issues can be clear. Whether it’s a singular “Big T” trauma or a series of less severe “Little T” traumatic events, the link between these experiences and a person’s behaviors can often be made easily. For example, a 58-year-old man who recently went through a divorce, was laid off and then lost his house, might make the connection between these experiences and his increased drinking and isolation.
However, the link between ACEs and mental health or substance abuse issues that develop later in life can be more difficult, for a couple of reasons. For one thing, the mental health or substance abuse issues often don’t surface until years, or even decades, after the Adverse Childhood Experience occurs. What starts as general family dysfunction, divorce, neglect, or abuse may seem relatively normal through childhood and even into adulthood. The early signs and symptoms of a greater issue often manifest themselves as isolation, lack of trust, avoidance and other social and emotional issues before they ever develop into substance abuse or severe mental illness.
What are ACEs?
The notion of Adverse Childhood Experiences, or ACEs, began with the research of the CDC-Kaiser Permanente Adverse Childhood Experiences (ACE) Study. The study was conducted between 1995 and 1997 and studied nearly 17,000 Kaiser patients in a San Diego Health Clinic[1]. Patient health was studied through physical exams and surveys of current health and behaviors, while they also completed surveys about childhood experiences. What this groundbreaking study was looking at was the link – which was not understood at the time – between childhood trauma and physical, mental and emotional health later in life.

The ten childhood experiences they were looking at were:
| Childhood abuse | 1. Emotional Abuse
2. Physical Abuse 3. Sexual Abuse |
| Childhood neglect | 4. Physical Neglect
5. Emotional Neglect |
| Household challenges | Growing up in a household were there was:
6. Substance abuse 7. Mental Illness 8. Violent Treatment of a mother or step-mother 9. Parental Separation/divorce 10. An incarcerated household member |
Participants in the study were then given an ACE Score between 0 and 10, the total sum based on how many of the 10 types of adverse experiences they reported experiencing.
The Findings of the CDC-Kaiser ACE Study
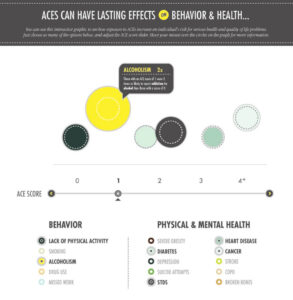
The ACE Score, from 0 to 10, is used to assess cumulative childhood stress – now sometimes referred to as “Little T” trauma or by association with this study – a person’s “ACEs”. One of the clearest and most widely understood finding of the study was that Adverse Childhood Experiences (ACEs) are more common than one might think, or thought at the time. More than half (52%) of the participants from the original CDC-Kaiser study reported having at least one ACE, and more than 1 in 5 (20%) reported exposure to 3 or more ACEs, while another 6.2% reported 4 or more exposures[2].
The most prevalent of the categories of childhood exposure was substance abuse in the household (25.6%); the least prevalent exposure category was evidence of criminal behavior in the household (3.4%)[3]. Another finding was that the susceptibility of a person’s exposure to multiple ACE categories, as the relationship between single categories of exposure was significant. If someone reported any single category of exposure, the probability of exposure to any additional category ranged from 65%–93%; and then not surprisingly, the probability of more than two additional exposures ranged from 40%–74%[4].
The key finding of the study as it related to health outcomes, and which changed the way we understood childhood trauma, was that as one’s ACE Score increases, so does the risk for serious diseases and conditions, including:
- Alcoholism and alcohol abuse
- Illicit drug use
- Depression and other mental health issues
- Suicide attempts
- Health-related quality of life
- Smoking
- Chronic disease
- Heart and liver disease
- Poor academic achievement
- Poor work performance and financial stress
- Risk for intimate partner violence
- Multiple sexual partners
- STDs and unintended pregnancies
- Risk for sexual violence and intimate partner violence
The increased risk for these negative health outcomes and well-being are dramatic. Compared to someone with an ACE Score of 0, a person with an ACE Score of 4 or more is:
- 18 times as likely to have attempted suicide
- Twice as likely to have had two or more weeks of depressed mood in the past year
- Nearly 5 times as likely to have ever used illicit drugs
- More than 11 times as likely to have ever inject drugs
- More than 5 times as likely to be an alcoholic
How are ACEs Linked to Health Issues?
There is a large and growing body of research about how childhood stress and trauma affect brain development, brain chemistry and, thus, the regulation of the body’s emotional, stress and fear response systems are impacted. Repeated stress and activation of these systems of the brain dramatically alter the formation of myelinated axons and the amygdala, the part of the brain that activates the autonomic nervous system (ANS) and releases hormones like adrenaline and cortisol into the body. If you’re walking through the woods and see a bear approaching, or you see a kid walking into oncoming traffic, the activation of this system is very effective in increasing your heart rate, opening your airways, and increasing blood flow to your organs and muscles, and away from certain parts of the brain.
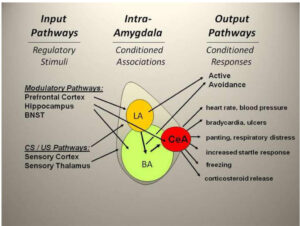
However, if the stress response system is activated every night by the sound of your dad coming home, or the sight of your mom reaching for a bottle of alcohol, your body and brain are hit with the same fight-flight-freeze response. The repeated activation of this system take a toll on your vital organs as well as your brain’s ability to regulate emotions and responses to triggers. When the body produces too much of, or stops producing, the natural chemicals to sooth or excite you, it is very common for people to turn to external stimuli to compensate this: depressants like alcohol and benzodiazepines, stimulants like cocaine and methamphetamine, or even behaviors like gambling and sexual intercourse.
Exposure to abuse and neglect also impact the prefrontal cortex, the part of the brain responsible for high level cognition and controlling impulse, and the nucleus accumbens, the brain’s pleasure-reward center which releases the body’s natural dopamine. The nucleus accumbens was first discovered in 1954 by two scientists when rats became addicted to pressing a lever that activated this part of the brain. The role of the nucleus accumbens and its connection to the amygdala and hippocampus[5] have great implications in the study of psychiatric disorders, substance abuse and addiction, obsessive compulsive disorder and Tourette’s Syndrome, and more studies are being conducted.
Dose-Response Relationship
The CDC-Kaiser study also found a “dose-response” relationship between ACEs and negative health and well-being outcomes across a person’s lifetime. A dose-response relationship is one where as the dose or intensity of the trigger increases, so does the intensity of the maladaptive behavior or response. For example, the more a person is exposed to abuse or neglect, the more severe the negative health outcomes will be.
Follow-Up Studies
Dr. Nadine Burke-Harris
One of the most notable cases of these results in action was the work of Dr. Nadine Burke-Harris, a pediatrician in San Francisco who was originally unaware of the CDC-Kaiser ACE Study. She noticed when she began working in a hospital in Bayview-Hunter’s Point, a low-income area of the city riddled with addiction and violence, that there was an abnormal number of children being referred to her for Attention Deficit Hyperactivity Disorder (ADHD). One of her colleagues made her aware of the ACE Study, which led her down a path of studying her patients’ exposure to trauma and how the brain and body were impacting their health. She subsequently started the San Francisco Center for Youth Wellness, where Dr. Burke-Harris made it routine to screen children for their ACE Score to better understand the risk factors of these youth across their lifetime.
See her TED Talk on How Childhood Trauma Affects Health Across a Lifetime:
Behavioral Risk Factor Surveillance System (BRFSS)
In 2009, the CDC began collecting annual ACE data through the Behavioral Risk Factor Surveillance System (BFRSS) from voluntary respondents telephonically. It is now the longest-running phone survey in the world. The BFRSS asks questions modified from the original ACE Study, from people across 32 states, using randomly dialed numbers. The data collected from the BRFSS are:
All ACE questions refer to the respondent’s first 18 years of life.
- Abuse1
- Emotional abuse: A parent or other adult in your home ever swore at you, insulted you, or put you down.
- Physical abuse: A parent or other adult in your home ever hit, beat, kicked or physically hurt you.
- Sexual abuse: An adult or person at least 5 years older ever touched you in a sexual way, or tried to make you touch their body in a sexual way, or attempted to have sex with you.
- Household Challenges
- Intimate partner violence:2 Parents or adults in home ever slapped, hit, kicked, punched or beat each other up.
- Household substance abuse: A household member was a problem drinker or alcoholic or used street drugs or abused prescription medications.
- Household mental illness: A household member was depressed or mentally ill or a household member attempted suicide.
- Parental separation or divorce: Parents were ever separated or divorced.
- Incarcerated household member: A household member went to prison.
The findings of the BFRSS are similar to that of the original CDC-Kaiser ACE Study:
- More than two-thirds of the participants reported at least one adverse childhood experience
- More than 1 in 5 reported exposure to 3 or more ACEs
Similarly, they also found a dose-response relationship with ACE Scores correlated to an increase in the following:
- Myocardial infarction
- Asthma
- Mental distress
- Depression
- Smoking
- Disability
- Reported income
- Unemployment
- Lowered educational attainment
- Coronary heart disease
- Stroke
- Diabetes
Treatment of Childhood Trauma
Understanding the role that adverse childhood experiences (ACEs) play in brain development and prevalence of addiction, mental illness and life-threatening diseases is a pivotal precursor to addressing these issues. Identifying and acknowledging the root of the issues is an important step in the recovery process, and only once a person can work through the lasting effects of exposure to Adverse Childhood Experiences can they truly recover. Because of the way these experiences embed themselves in our brain and body, the process of resolving them can take months or even years, but even the most complex trauma can be resolved with enough time and commitment.
Despite the acceptance of this research in the medical field, behavioral health professionals have been slower to integrate the identification and treatment of trauma into practice. It is important for someone who has been exposed to these adverse childhood experiences to find help at trauma-focused treatment programs like Roots Through Recovery, who utilize evidence-based approaches like Eye Movement Desensitization and Reprocessing (EMDR), Somatic Experiencing (SE), Mindfulness-Based Stress Reduction (MBSR), Trauma-Focused Cognitive Behavioral Therapy (TF-CBT), and expressive approaches like music and sound therapy, trauma-focused yoga, and art therapy.

Resources:
[1] https://www.ajpmonline.org/article/S0749-3797(98)00017-8/fulltext
[2] https://www.ajpmonline.org/article/S0749-3797(98)00017-8/fulltext
[3] Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. https://www.ajpmonline.org/article/S0749-3797(98)00017-8/fulltext
[4] https://www.ajpmonline.org/article/S0749-3797(98)00017-8/fulltext
[5] https://www.eurekalert.org/pub_releases/2014-05/cafn-itp052114.php




